Patient: Peter Smith
Social security number: 110350-1O3N
Diagnosis: Infarctus cerebellum 25.11.2014
Background information
The patient is a computer teacher and two days ago he felt dizzy and sick at home and fell down on the floor. His sister called for an ambulance and the patient was taken to the central hospital. Thrombolytic care was given within three hours of the first symptoms. The patient is now in the stroke unit. He has no hemi paretic nor sensory symptoms, but he has a strong pusher syndrome on the right side and he cannot control his sitting and standing position.
I ask politely to start mobilizing according to the condition of the patient.
Neurologist Joe Bratt
Neurological department doctor
- What do you want to know about Peter’s background and why? What is important if you want to plan therapy which is based on neural plasticity and patient’s active role? Make questions, Peter will answer you.
It is important to know general information about the study case, patient’s background (past medical history), patient’s condition before incident and patient’s current state/condition.
General information:
How old are you?
What is your current profession?
Do you smoke/drink?
What are the activities/hobbies that you enjoy?
Past medical history:
Do you take currently medication?
Have you been to a physiotherapist for any conditions? What were they?
What examinations have you done?
Did you already have a stroke?
Somebody in your family had a stroke?
Patient’s condition before incident:
Can you describe what happened before your fall?
When was your last fall in the last 6/12 months except this one?
Do you often practice a sport?
Do you live alone?
What is the layout of your home/office?
Patient’s current situation:
How are you feeling now?
On a scale from 1 to 10, how much is your pain? How would do describe it?
Are you experiencing any numbness or loss of sensation?
Do you have expectations about physiotherapy?
Regarding neural plasticity and patient recovery, the functional part before the accident is important to take in consideration. In order to promote high motivation from the patient and a potential increasement of neural plasticity, it should be important to identify an activities/hobbies enjoyable for the patient.
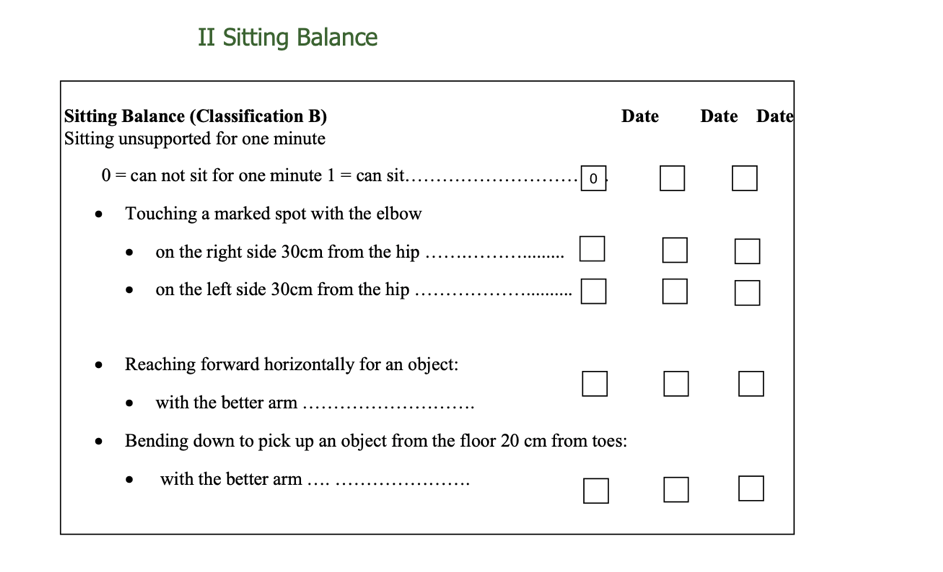
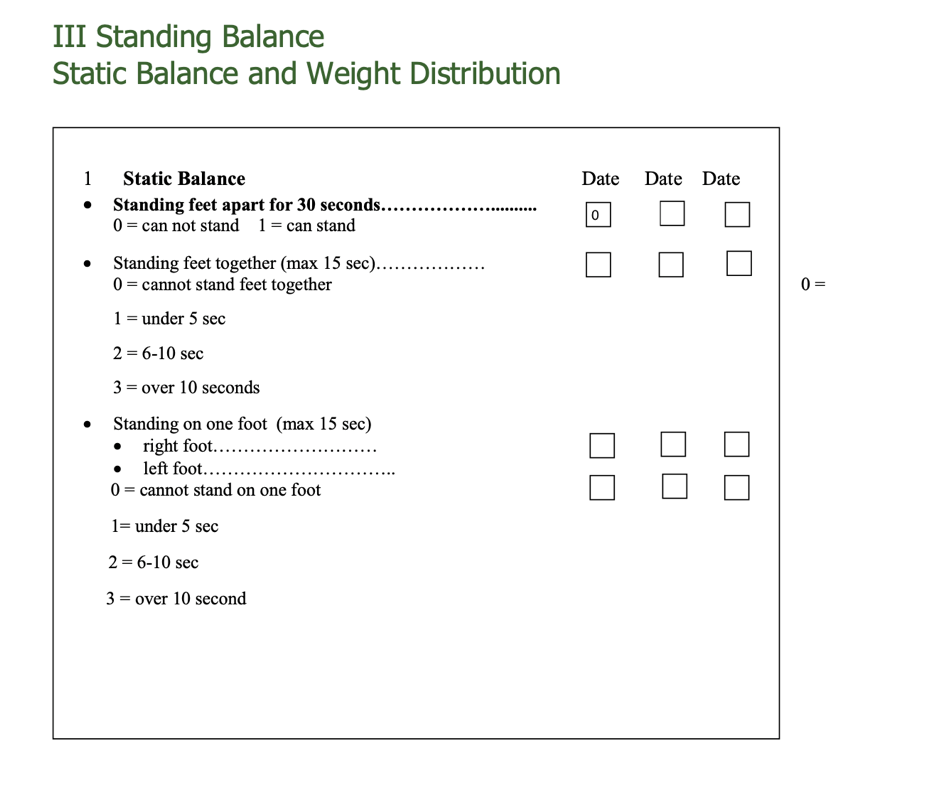
- Watch the following video and measure Peter’s postural changes and his sitting and standing balance after 6 days post stroke by using the PCBS test. Give the points and write a short summary about his balance ability. Peter’s PCBS test 6 days after stroke
For this task use the PCBS test form below.

Regarding postural changes, the patient is independent but show signs of decreased control (16 point or classification 2). In position requiring vertical positioning, the patient demonstrate pushing on the right side.

Regarding sitting balance, the patient was unable to stay 1 minute sitting without assistance (0 point). The subsequent tests were not tested. The patient indicates a pushing syndrome on the right side.
Regarding standing balance, the patient is not able neither standing up 30 seconds without assistance (0 points). The subsequent tests were not tested. The patient points more weight out on the right/non-affected side.
- What other kind of knowledge about patient’s functional capacity do you need in the acute phase of stroke? Read the following studies and pick up then most important things, that should be considered. Then make a summary about elements which are important to be followed up in the acute phase of stroke.
Upper limb: Fugl-Meyer motor evaluation, grip function
In case of flaccid upper limb, it could be important to evaluate the patient through Fugl-Meyer motor evaluation within 4 weeks after onset in order to have an optimal prediction of arm function outcome at 6 months. It demonstrates that lack of voluntary motor control of affected leg without any synergic movement of the affected arm is associated with a poor outcome at 6 months. Otherwise, there is 74% chance of regaining some dexterity. The absence of a measurable grip function at 1 month after stroke was found to be indicative of a poor functional recovery of the hemiplegic arm, whereas early return of voluntary motion of paretic arm within the first weeks after stroke is considered to be a good prognostic sign.
Gait assessment: sitting balance and muscle strength of paretic leg
The first goal in stroke rehabilitation is to regain independent gait. Accurate prediction within 72 hours is attainable at hospital stroke units by means of 2 simple bedside tests: sitting balance and muscle strength of the paretic leg.
Those non-ambulatory patients who regained their sitting balance as assessed by the trunk control test and developed some voluntary movement of the hip, knee, and/or ankle as assessed by the motricity index leg score (≥25 points) within the first 72 hours post-stroke had about a 98% chance of regaining independent gait within 6 months. In contrast, those patients who were unable to sit independently for 30 seconds and were not or hardly able to contract the muscles of the paretic lower limb within 72 hours had a probability of about 27% of achieving independent gait. Patients with a poor prognosis should be reassessed with these 2 tests on day 9 to improve the accuracy of prediction.
Improvement in standing balance control is more important than improvement in leg strength or synergism to achieve improvement in walking ability, whereas reduction in visuospatial inattention is independently related to improvement of gait. Recovery in postural control of standing is more important for regaining gait than the restoration of support functions and voluntary control of the paretic leg itself.
Daily routine: Bartel Index, NIHSS, Canadian Neurological Scale
Day 5 after stroke proved to be the earliest time for making an optimal prediction at 6 months of final outcome of activities of daily living. The BI should be measured at the end of the first week in hospital-based stroke units for early rehabilitation management.
Assessment on Day 2 resulted in an increased number of false-negatives and consequently an underestimation of the final outcome of activities daily living, whereas assessment on Day 9 resulted in a relatively overestimation of the final Barthel Index at 6 months.
The accuracy of the NIHSS in predicting ADL outcome is almost unaffected by the timing of assessment in the first 9 days after stroke, making this instrument more robust for determining patient prognosis.
Strong evidence that age and outcomes assessing severity of neurological deficits in the early post stroke phase, such as the NIHSS and Canadian Neurological Scale, are highly associated with final basic activities daily living outcome beyond 3 months after stroke. In addition, there is strong evidence that gender and the presence of risk factors for stroke, such as atrial fibrillation, do not predict outcome of basic activities daily living.
Prediction of walking ability and functional independence during one week after stroke (Woldag et al 2006, Kollen et al 2005)
Prediction of gate within 72 hours post stroke (Veerbeek et al 2011)
Prediction of the recovery of the upper limb in the acute phase of the stroke ( Nijland et al 2010, Kwakkel et al 2003)
Predictors for outcome of ADL after stroke (Veerbeek et al.2011)
The Barthel Index as predictor of activities of daily living outcome after stroke (Kwakkel et al 2011, De Wit et al 2014)